In addition to animal tissue, human placental tissue offers great advantages as a tissue source due to its human origin, molecular composition, and availability as a clinical waste product.

In our studies, human placental arteries were decellularized and showed low immunogenicity and favorable conditions for cell migration and proliferation. In addition to its application as a small-lumen vascular graft substitute, placental tissue could also be a useful biomaterial source for other applications in regenerative medicine. We have developed an ECM hydrogel from human placental tissue with very good cytocompatibility and immunomodulatory capacity. Currently, this material is being investigated as 3D printed ECM scaffolds and as an injectable hydrogel for various cardiovascular applications.
Ongoing Projects

Materials derived from nature offer many mechanical, chemical, and biological advantages over synthetic materials. Their application requires a preservation method that could remove immunoreactive binding sites while maintaining the mechanical integrity and natural compliance of the scaffolds. In this project, allogeneic or xenogeneic arteries from various donors will be investigated as bio-prosthetic vascular graft substitutes. The tissues will be treated with different methods to digest cells and cell-associated antigens. Biomaterials derived from allogeneic human cadaveric donors raise ethical concerns. Tissues derived from animal sources are xenogeneic materials and may be contaminated with pathogeneic prions. Therefore, vessels from human placenta and umbilical cord are currently being investigated for their potential as vascular graft substitutes.
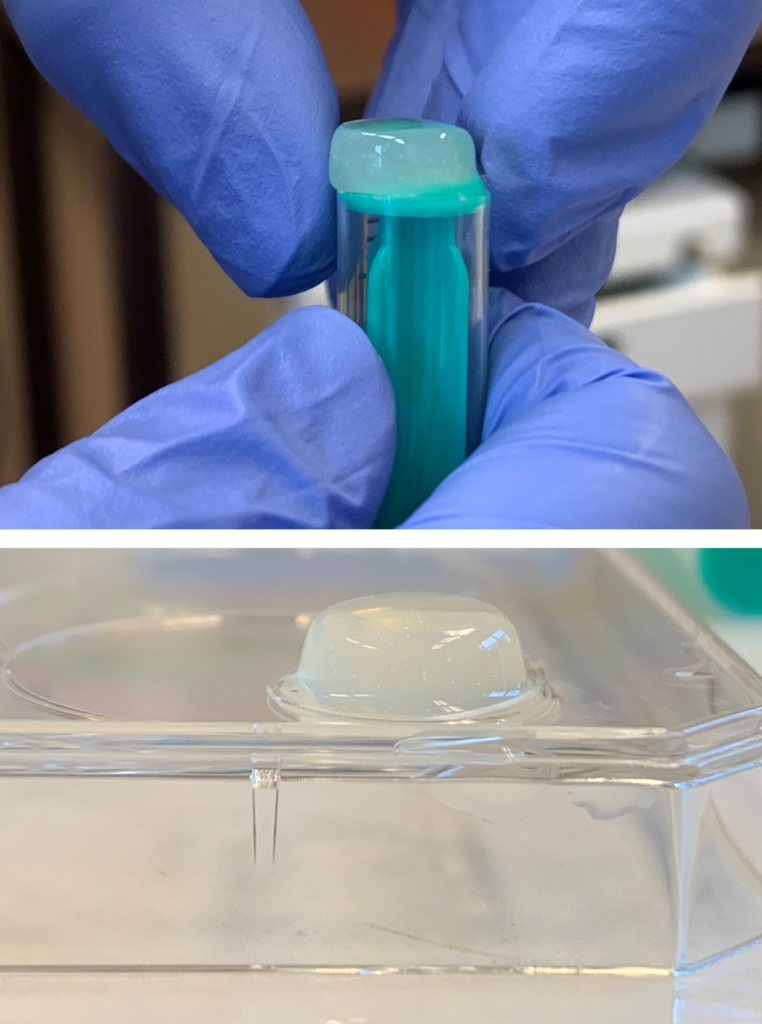
Hydrogels, which are made from biological tissue, are becoming increasingly important for regenerative medicine due to their structure and wide range of applications. Besides in vitro application, hydrogels can be used as for 3D printed implants, as coatings for prosthetic materials and as injectable biomaterials to improve functional tissue regeneration in wounds and necrotic tissue. We produce hydrogels from various tissue types such as human placenta or porcine hearts. The hydrogels are studied in detail with respect to their molecular composition, biocompatibility and biomechanical properties. Optimized hybrid gels are currently being tested for their applicability as injectable or 3D-printed scaffolds for tissue regeneration after myocardial infarction.
